(This article is reproduced from Science Monthly: https://www.scimonth.com.tw/archives/10955)
author: Cheng-Chih Hsu / Associate Professor of the Department of Chemistry at National Taiwan University, founder and CEO of Leeuwenhoek Biotech; currently a director of the Taiwan Society of Mass Spectrometry, specializing in analytical chemistry and biomedical mass spectrometry.
If you haven’t heard of the famous “slimming pen” Saxenda, then you are really out of date! In recent years, the global biotech industry and capital markets have been frantically pursuing weight-loss drugs like SanofiZa. Here are some recent news headlines
•《Business Times》 (May 25, 2023): "The share price of Novo Nordisk, the Danish pharmaceutical company that developed the injection, has soared 40% in the past six months, with a market value of US$326 billion, making it the world's second largest pharmaceutical company."
• "This Week" (December 13, 2023): "According to Citi analysts' forecasts, by 2035, annual revenue from weight loss drugs is expected to reach $71 billion, and Barclays is more optimistic about reaching $100 billion."
Next, let us introduce these "glucagon-like peptide-1" (GLP-1), which has created a lot of topics and is the most popular in the pharmaceutical industry!
The function and application of GLP-1 in helping the body lower blood sugar
Although the Slim Pen looks a bit like an insulin injection pen, it is actually a polypeptide drug with the scientific name liraglutide, and is also a chemically modified analog of GLP-1.
GLP-1 is a polypeptide hormone incretin secreted by specific intestinal cells (L cells). After eating, GLP-1 can promote insulin secretion to regulate blood sugar concentration. Fats, proteins, and carbohydrates in food can induce L cells to secrete GLP-1, which is then transported to the pancreas via the blood, thereby stimulating insulin secretion and inhibiting glucagon concentrations to lower blood sugar. The above mechanism is the function of GLP-1 that was first understood in the medical field. Therefore, the GLP-1 drugs developed at the beginning were mainly used to treat type 2 diabetes. This type of drug is also called GLP-1 receptor agonist.
However, the half-life of GLP-1 is very short, only about two minutes, mainly because it will be broken down by the DPP4 (dipeptidyl peptidase-4) enzyme that is prevalent in the body, preventing the body from accumulating too much GLP-1 and affecting other important physiological functions. If we synthesize a peptide that is exactly the same as the endogenous GLP-1 secreted by the body, the fate will be the same as the endogenous GLP-1 peptide. It will be degraded by the body's enzymes within two minutes in the blood, and therefore cannot be used as a drug. Therefore, how to modify GLP-1 by chemical modification to produce a drug with the same function that can act in the body for a long time has become an important issue in using GLP-1 to control blood sugar in patients with type 2 diabetes or to suppress appetite.
Liraglutide, launched by Denmark's Novo Nordisk Pharmaceuticals, has made some minor changes or modifications to the amino acid sequence of human GLP-1. During the research and development process, scientists must first determine which positions cannot be touched. The affinity between the drug and the corresponding receptors on the cells cannot be lost, but the affinity cannot be too high, which would hinder GLP-1 from performing its task and turn it into an antagonist. Then they begin to fatten the positions that can be moved to prolong the blood circulation time of the polypeptide. Fatty acids not only slightly increase the steric hindrance of degradation, but also tightly bind the fatty polypeptide to albumin. Therefore, the time it takes to be degraded by half in the body is prolonged, and it can be released slowly in the blood.
The fat-modified liraglutide still has about 97% similarity with the human GLP-1 amino acid sequence, but the time it takes to be degraded by the DPP4 enzyme in the body has increased significantly from the original two minutes of endogenous GLP-1 to 13 hours. The newer version of the GLP-1 peptide analog Ozempic (semaglutide) extends the time it takes to be degraded by half to one week, so semaglutide has also been approved for the treatment of type 2 diabetes.
GLP-1 and weight loss
In addition to being distributed in the pancreas, GLP-1 receptors are also found in the stomach and central nervous system. Stimulation of the GLP-1 receptors here has the effect of slowing down gastric emptying, suppressing appetite and increasing satiety. These characteristics are also used by pharmaceutical companies in the development of weight-loss drugs. In a large-scale clinical trial, it was found that subjects treated with liraglutide lost an average of about eight kilograms in one year, while the control group only lost about three kilograms. Statistical analysis has proven the weight-loss effect of liraglutide, making it a hot topic in the global pharmaceutical industry. Currently, most people who take liraglutide do so not to treat type 2 diabetes, but simply to lose weight.
Although the slim pen is known as a magic drug for weight loss, the use of GLP-1 receptor agonists also has side effects, the most common of which include nausea, vomiting, and diarrhea. The most likely cause of these side effects is overstimulation of the central nervous system. Therefore, the quality of life of patients treated with GLP-1 receptor agonists may still be affected, and successful weight loss is not a permanent solution, and they may gain weight again after stopping the drug.
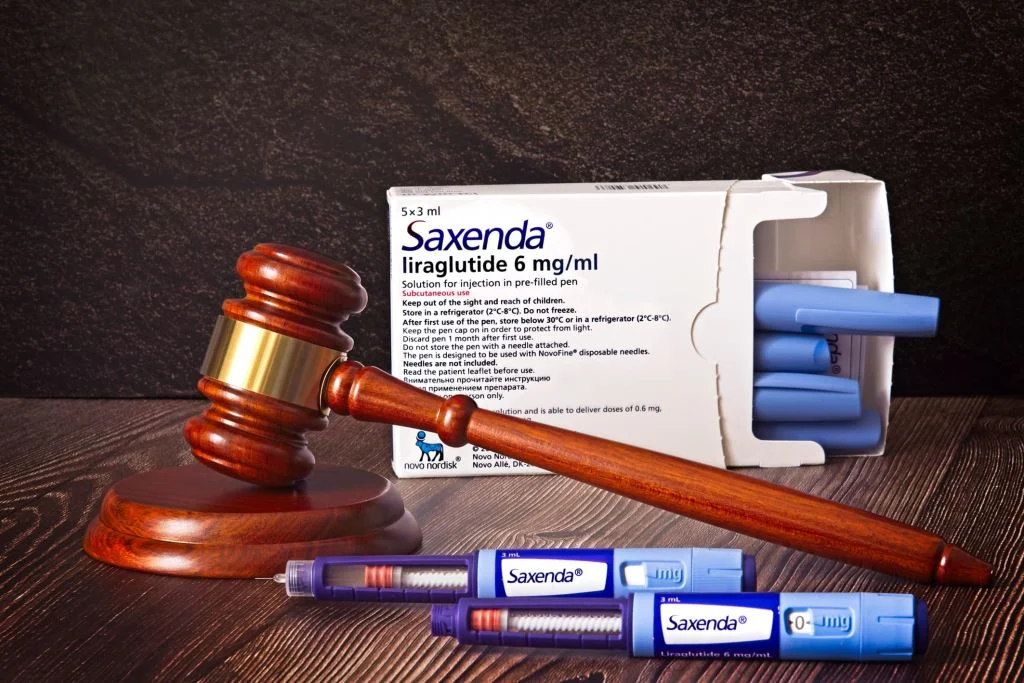
(Photo: Adobe Stock)
To reduce side effects, start with intestinal bacteria?
Studies in recent years have shown that intestinal flora is correlated with the occurrence of many diseases, including diabetes and obesity mentioned in the previous two paragraphs. GLP-1 is secreted from intestinal cells. Intestinal bacteria living in the gastrointestinal tract will of course affect the secretion of GLP-1. It is currently known that intestinal bacteria produce many small molecule metabolites that promote GLP-1 secretion, such as short-chain fatty acids, secondary bile acids such as acetate, propionate, butyrate, and tryptophan metabolites. In addition to these small molecule metabolites, some intestinal bacteria also secrete specific peptides that stimulate intestinal L cells to secrete GLP-1.
In addition, Akkermansia muciniphila (AKK), the next-generation probiotic that is currently receiving the most attention, has been shown in animal experiments to improve obesity and type 2 diabetes and promote intestinal barrier function. A study in 2021 found that AKK also promotes the secretion of GLP-1. After 14 weeks of giving obese mice live AKK bacteria, the concentration of GLP-1 induced by drinking sugar water in the blood of mice that consumed live AKK bacteria daily was higher than that of mice that did not consume live AKK bacteria. Obese mice that consumed live AKK bacteria weighed less and had better blood sugar regulation than mice that did not consume live AKK bacteria. In this study, it was discovered that AKK secretes a peptide named P9. In addition to stimulating L cells to secrete GLP-1, the P9 peptide can also reduce the body weight of obese mice and improve blood sugar regulation.
Although more clinical trials are needed to prove this, current research by teams around the world shows that the endogenous GLP-1 secreted from the intestine has a more "natural" structure and does not exist in the body for as long as GLP-1 receptor agonists. Therefore, some people have suggested that by changing the intestinal flora to promote the secretion of GLP-1, there is a chance to reduce the occurrence of side effects such as nausea, vomiting, and diarrhea. In addition, some foreign manufacturers have combined multiple probiotics, including AKK that produces P9 and propionic acid, Clostridium butyricum and Bifidobacterium infantis that produce butyric acid, to launch probiotic products that claim to increase GLP-1 secretion.
Future development trend of GLP-1 products
Nowadays, in addition to GLP-1 receptor agonists, some teams are also developing weight loss therapies combined with other incretin receptor agonists. Current clinical trial results show that GLP-1 receptor agonists combined with other incretin agonists have a better weight loss effect. For example, Eli Lilly has launched trizepatide, a single molecule that can activate both GLP-1 receptors and gastric inhibitory polypeptide (GIP) receptors. However, like other GLP-1 receptor agonists, common side effects of trizepatide include nausea, diarrhea, and indigestion. Many of these modified "non-natural" GLP-1s have gradually lost public attention due to cases of serious side effects.
At the same time, there is increasing evidence that intestinal bacteria can promote the secretion of natural GLP-1 and other intestinal secretins, such as GIP, in the intestine. This also suggests that if the intestinal flora can be changed, there will be an opportunity to create a so-called "lean body" to make the weight loss effect more lasting and save patients from the uncomfortable side effects of using weight loss drugs.
If the intestines are healthy, the person is healthy. Let us look forward to the continuous advancement of science so that humans can one day live to be 100 years old!



