
To become beautiful, start with adjusting the intestinal environment – Talking about the butterfly effect of the gut-skin axis
"If you have acne, eat less fried food" and "Avoid sugar and dairy products to avoid acne" - these seemingly simple beauty tips actually contain a neglected health clue:The deep connection between the intestine and the skin. Many studies have confirmed that the health of the intestines not only affects digestion, but also affects Gut-skin axis Affects the skin's inflammatory response, barrier function and oil secretion. If you want to truly improve your skin quality and restore it to a stable and translucent state, you should start by conditioning your intestines.Systematic maintenance"The original starting point."
One gatekeeper inside and one outside: The intestine and skin are actually "twin organs"
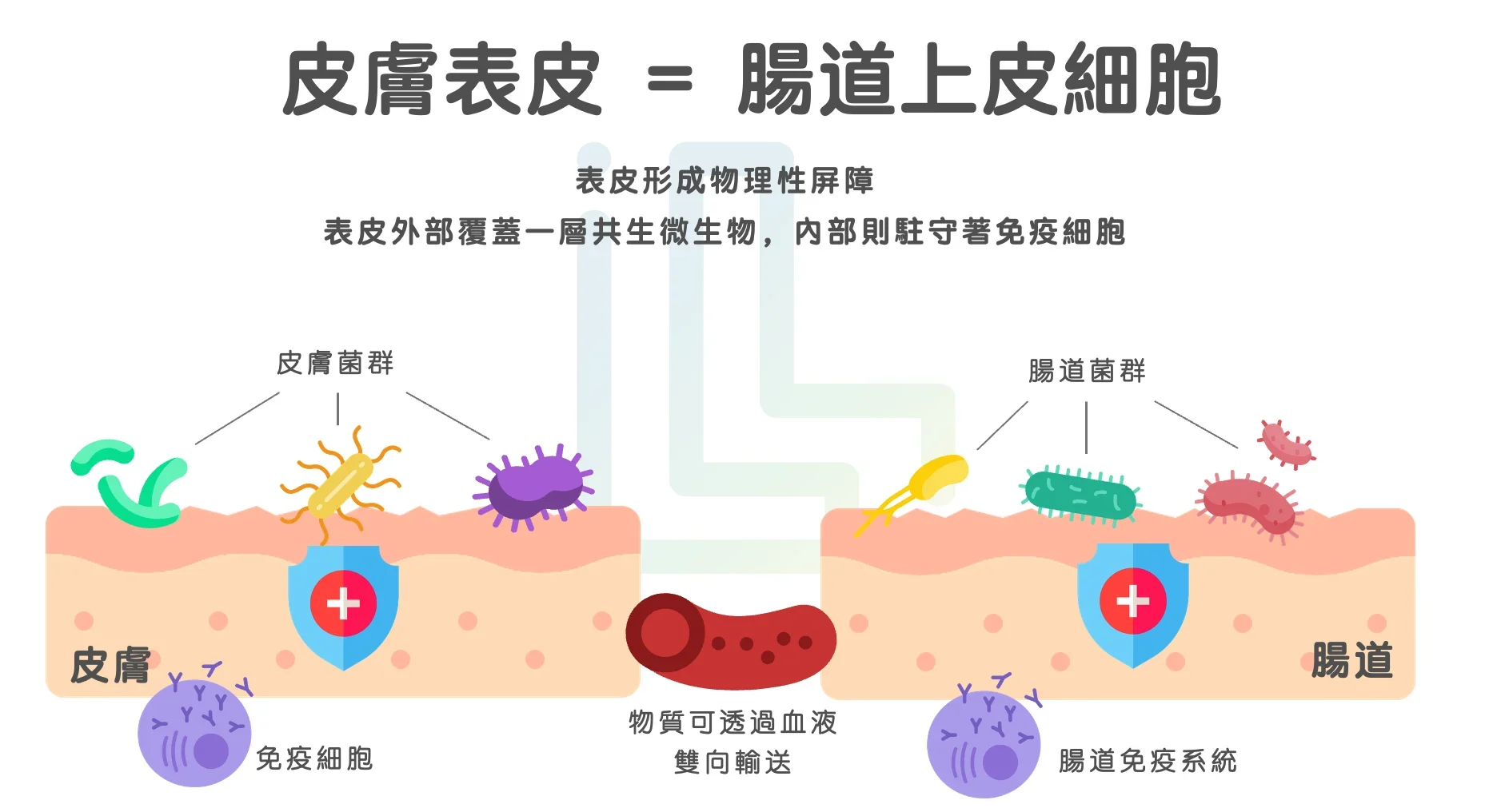
The intestine and skin are two important contact organs of the human body. In the human body, the intestines and skin face inwards and outwards respectively, but they have similar tasks: they are both our connection to the outside world.Barrier system.Skin is the gatekeeper to the outside world, block germs, dust and ultraviolet rays at the first time (And the PM2.5 that has been making a lot of noise lately);The intestine is the body's filtration station, which is not only responsible for nutrient absorption, but also prevents harmful substances from entering the blood.
The two organs have more in common than that. The skin and the lining of the intestine are covered withMicrovessels and immune cells, establishing deep connections with each other through immune signaling, neural regulation and microbial metabolites. This interaction is calledGut-Skin AxisIt is not just a collaboration between organs, but also a movement from within.Microvessels and immune cellsA coordinated defensive action that impacts systemic skin condition. In other words, when the intestinal tract is not in good condition, the skin will also be affected.
The gut-skin axis in a healthy state: harmonious functioning of the internal and external barriers for a naturally radiant complexion
In an ideal intestinal state, the flora is rich in diversity, the good bacteria and bad bacteria are balanced, and the intestinal barrier function is sound. In this state, the good bacteria in the intestine (for example:Bifidobacterium, Lactobacillus) will produce some products with health functions (Metabolites, also known as postbiotics), such as:
- Short-chain fatty acids (SCFAs): It has the ability to resist inflammation, maintain immune function, and promote barrier repair.1
- Indole metabolites (eg, indole-3-propionic acid, IPA): Helps to resist oxidation and stabilize immune function.2
In this ideal state, not only is the intestine healthy, and inflammation and flatulence are not likely to occur, but these good metabolites can also be transmitted to the skin through the gut-skin axis, reducing the skin's inflammatory signals, balancing the secretion of moisture and oil, and the overall skin condition will be stable (Occasionally eating fried food will not cause acne to break out immediately), Bright (The complexion is naturally bright and not dull),meticulous(Acne and pores are less noticeable).
In short, you can go out without makeup 🙂
Unbalanced gut-skin axis: Civil war breaks out, and the outer line is also lost
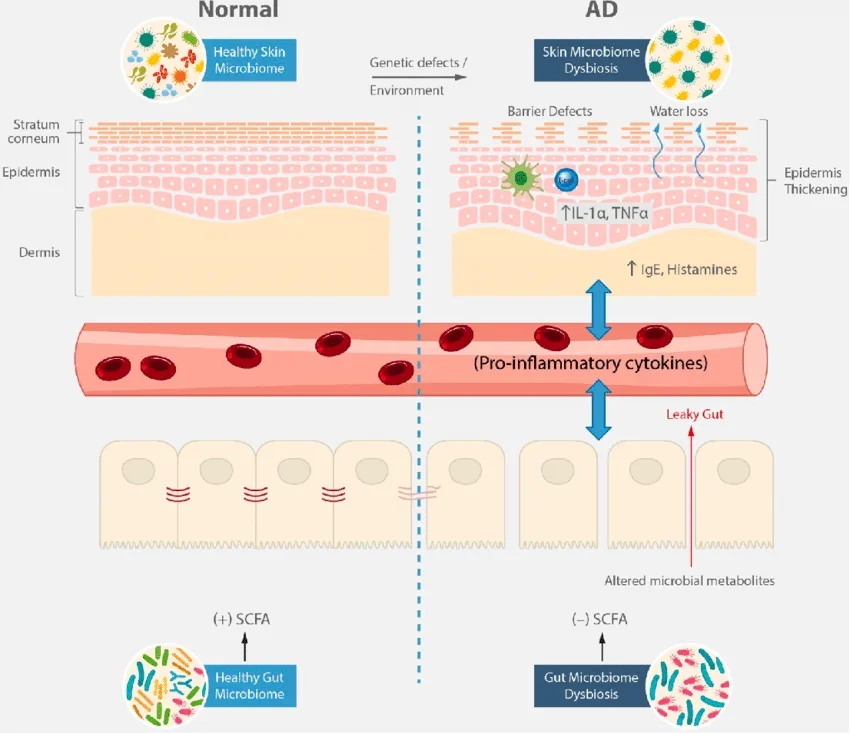
However, modern peopleLong-term stress, with a refined diet and a fiber-deficient lifestyle, the microbial ecology in the intestines is easily disrupted. When the intestinal flora is unbalanced, bad bacteria (especiallyGram-negative bacteria) will increase abnormally. They are bad because their cell walls containLipopolysaccharide (LPS), LPS is an endotoxin (The enemy during war), when it accumulates excessively in the body, it triggers a series of inflammatory responses.3
Of course, the human body is intelligent, so under normal circumstances, LPS should be confined to the intestines, so the inflammatory response will not spread to other parts of the body through the blood; but whenImpaired intestinal barrier function(Yes, it is also because of the reasons mentioned above), for example, the inhibition of tight junctions may lead toIncreased intestinal permeability(Broken gate concept), which is the so-called Leaky gut. Once the intestinal barrier collapses, just like a city gate is wide open, LPS can pass through the intestinal wall and enter the blood.It is delivered to various organs of the body through the microvessels covering the intestines, and the skin is the most obvious outlet.4
What skin problems may be caused by an imbalance in intestinal flora?
- Acne vulgaris:Changes in intestinal bacteria can trigger an inflammatory response. When a diet high in sugar, fat, and dairy products leads to leaky gut, endotoxins enter the blood circulation, stimulating sebaceous gland activity, increasing sebum secretion, and forming acne.5
- Atopic dermatitis:Atopic dermatitis is highly correlated with intestinal immune system dysfunction, mainly because bacterial flora imbalance reduces the immune regulatory ability of regulatory T cells (Treg), causing the body to lose tolerance to allergens and further induce systemic chronic inflammation.6
- Chronic sensitive skin and dry skin:Short-chain fatty acids (SCFAs) produced by beneficial intestinal bacteria are essential for maintaining the integrity of the skin barrier. In addition to affecting immunity, SCFAs can also improve the health of skin keratinocytes. If intestinal bacteria cannot effectively produce SCFAs, it will indirectly affect the health of the skin barrier.7
- Dull skin and aging: An imbalance in intestinal flora increases the release of free radicals, leading to chronic low-grade inflammation and oxidative stress, further accelerating collagen loss and skin aging.8
Don’t just focus on skin care: Create a systematic skin care strategy
Now that you know the close connection between the intestines and the skin, have you started to rethink the direction of your skin care routine?
In the next article, we will provide several practical methods based on scientific evidence to help you optimize your intestinal environment, cultivate a stable, healthy, and translucent skin condition from the root, and truly radiate brilliance from the inside out✨
References
- Parada Venegas D, De la Fuente MK, Landskron G, et al. Short Chain Fatty Acids (SCFAs)-mediated gut epithelial and immune regulation and its relevance for inflammatory bowel diseases. Front Immunol. 2019;10:277. doi:10.3389/fimmu.2019.00277 ↩︎
- Li J, Zhang L, Wu T, Li Y, Zhou X, Ruan Z. Indole-3-propionic acid improves the intestinal barrier by enhancing epithelial barrier and mucus barrier. J Agric Food Chem. 2021;69(5):1487–1495. doi:10.1021/acs.jafc.0c05205 ↩︎
- Zhao M, Chu J, Feng S, et al. Immunological mechanisms of inflammatory diseases caused by gut microbiota dysbiosis: A review. Biomed Pharmacother. 2023;164:114985. doi:10.1016/j.biopha.2023.114985 ↩︎
- Mohammad S, Thiemermann C. Role of Metabolic Endotoxemia in Systemic Inflammation and Potential Interventions. Front Immunol. 2021;11:594150. Published 2021 Jan 11. doi:10.3389/fimmu.2020.594150 ↩︎
- Sánchez-Pellicer P, Navarro-Moratalla L, Núñez-Delegido E, Ruzafa-Costas B, Agüera-Santos J, Navarro-López V. Acne, Microbiome, and Probiotics: The Gut-Skin Axis. Microorganisms. 2022;10(7):1303. Published 2022 Jun 27. doi:10.3390/microorganisms10071303 ↩︎
- Lee SY, Lee E, Park YM, Hong SJ. Microbiome in the Gut-Skin Axis in Atopic Dermatitis. Allergy Asthma Immunol Res. 2018;10(4):354-362. doi:10.4168/aair.2018.10.4.354 ↩︎
- Trompette A, Pernot J, Perdijk O, et al. Gut-derived short-chain fatty acids modulate skin barrier integrity by promoting keratinocyte metabolism and differentiation. Mucosal Immunol. 2022;15(5):908-926. doi:10.1038/s41385-022-00524-9 ↩︎
- Millman JF, Kondrashina A, Walsh C, et al. Biotics as novel therapeutics in targeting signs of skin aging via the gut-skin axis. Ageing Res Rev. 2024;102:102518. doi:10.1016/j.arr.2024.102518 ↩︎



